COVID-19 – How Does it Work?
Some more recent information has come to light about the novel Coronavirus that’s sweeping the world right now. The discussion around which receptors in the body the Coronavirus actually latches onto has become of key interest. And since it is now the main topic of conversation surrounding COVID-19, I want to break it down for you here.
Some background first: in order for a virus to affect a host, it has to be able to get into the body, it has to lock onto a particular cell receptor (like a lock and key – which lets it inside the cell), and then it has to replicate.
What many researchers discovered in the literature on SARS virus, aka Coronavirus, is that this particular type of virus matches the lock/receptor known as the Angiotensin Converting Enzyme II receptor – or the ACE-2 receptor. Now, you may be familiar with ACE-inhibitors and ARBs – these are medications often used to manage hypertension.
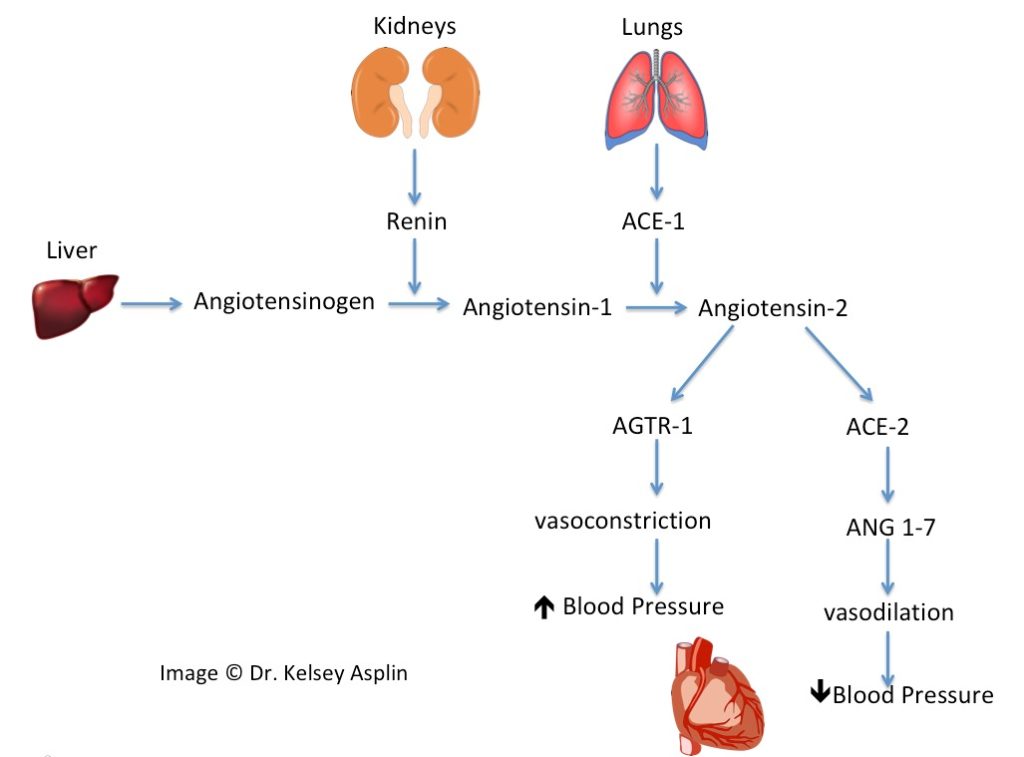
Let’s understand how the system normally functions:
- First, your innate blood pressure regulating system is called the Renin-Angiotensin-System (or RAS).
- Renin is released by the kidneys to convert Angiotensinogen (from the liver) into Angiotensin 1.
- Angiotensin-1 binds to Angiotensin Converting Enzyme (ACE) from the lungs, and become Angiotensin-2.
- Angiotensin-2 binds to its receptor, Angiotensin Receptor-1 (AGTR-1), and causes your blood vessels to constrict, which increases the force needed to pump your blood through the vessels, i.e. increased blood pressure. Think about switching to a smaller straw when you’re drinking a thick shake – you have to suck on the straw with more force to get the shake through it.
- Angiotensin-2 can also meet up with Angiotensin Converting Enzyme 2 (Enter: ACE-2) and turn into a different substance that actually opposes the effect of Angiotensin 2 and promotes vasodilation (think, switching back to a wider straw).
- These two options makes it possible for the body to control how constricted or dilated your blood vessels get, thereby creating a continuous ebb and flow of blood pressure intensity – all in an effort to maintain a balanced level.
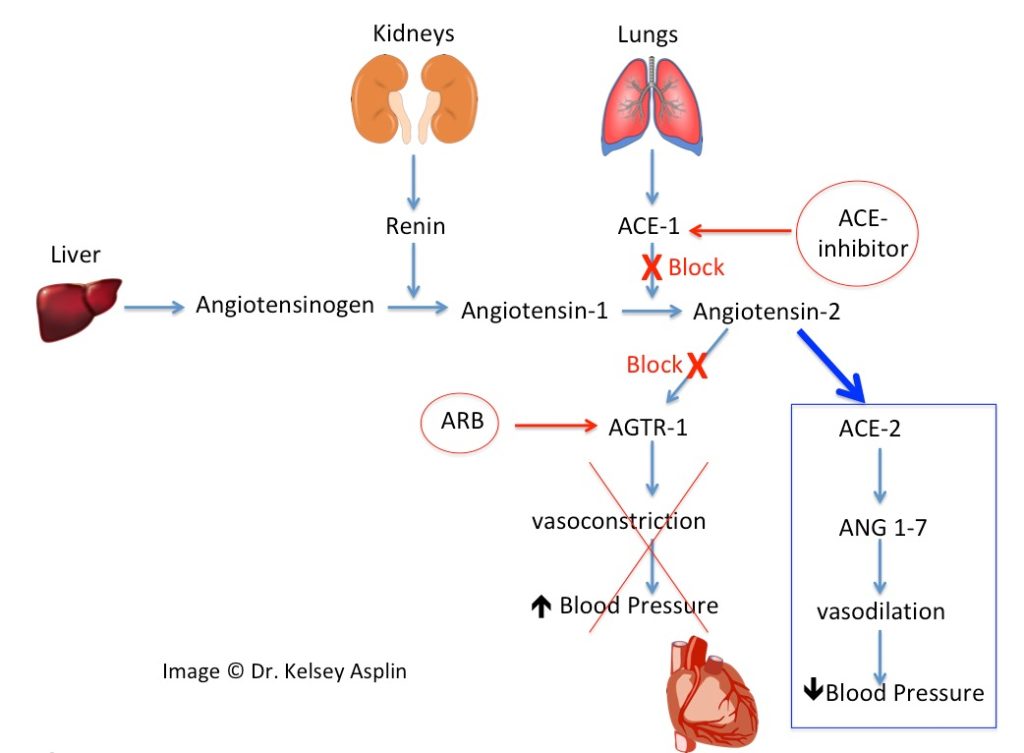
Now let’s understand how the medications work:
- ACE-inhibitors (aka angiotensin converting enzyme blockers), like Lisinopril, work in the body by blocking the conversion of Angiotensin-1 to Angiotensin-2.
- ARBs (aka angiotensin 2 receptor blockers), like Losartan and Valsartan, work by blocking the binding of Angiotensin-2 to it’s receptor, AGTR-1.
- If we block the conversion of Angiotensin-1 to Angiotensin-2, and block Angiotensin-2 from binding AGTR-1, then the arteries naturally relax and widen, which lowers blood pressure.
So, back to the ACE-2 receptor. These receptors predominate in the heart but are also found in the lungs, kidney, intestines – really all throughout the body. This may be the key to understanding why those with high blood pressure and other chronic health conditions, like diabetes and kidney disease, may be at higher risk if they “catch” the virus.
You see, when you take a medication that blocks a normal body process (like an ACE-inhibitor getting in the way of making Angiotensin-2 or an ARB getting in the way of Angiotensin-2 binding), the body tries to re-regulate by making more receptors that are available to bind to whatever small amount of Angiotensin-2 may be floating around the body (in this case, more ACE-2). The result is that a person taking these medications inevitably ends up with more receptors – which means more docking sites for the Coronavirus.
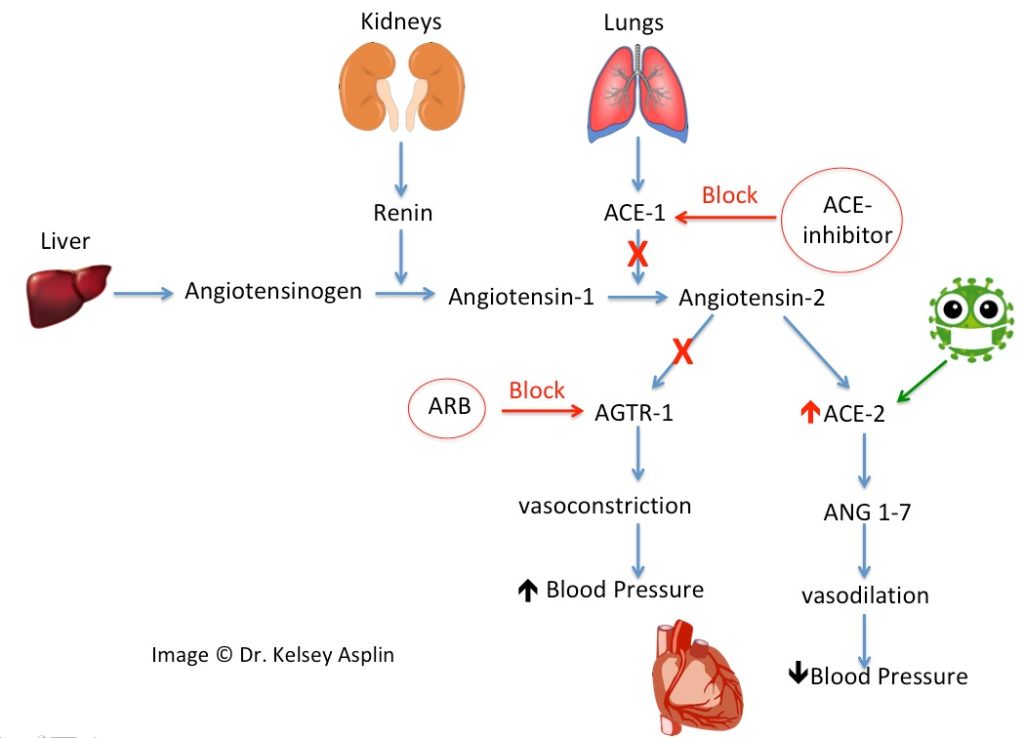
As an interesting side note, this may also be the reason behind patients continuously having to increase their blood-pressure medication doses.
Want more on how you can keep your defenses up? Check out our free guide for home-style immune support. Get it here!
Stay tuned, for as we learn more we’ll be passing it onto you.